Staphylococcus aureus infections affect up to 20% to 30% of the human population worldwide.
Staphylococcus is a family of bacteria, derived from the Greek word – Staphylo meaning grape-like, and coccus meaning berries. Sir Alexander Ogston discovered the Staphylococcus family in 1880 from pus in the injury. Later, Friedrich Julius in 1884, identified different species of Staphylococcus bacteria1. Staphylococcus aureus is a bacteria that render positive result on Gram stain test. Gram stain test is a common type of staining method to find out the presence of a particular species of bacteria.
According to a report published by Statens Serum Institut, Denmark, the Staphylococcus aureus infection in Denmark was in an increasing trend since 2001, and largely started to stay consistent since 2016. The similar situation can be observed in many other developing and developed countries1. Even though, the number of cases that occurred per year remained the same, the bacteria became resistant to more antibiotics.
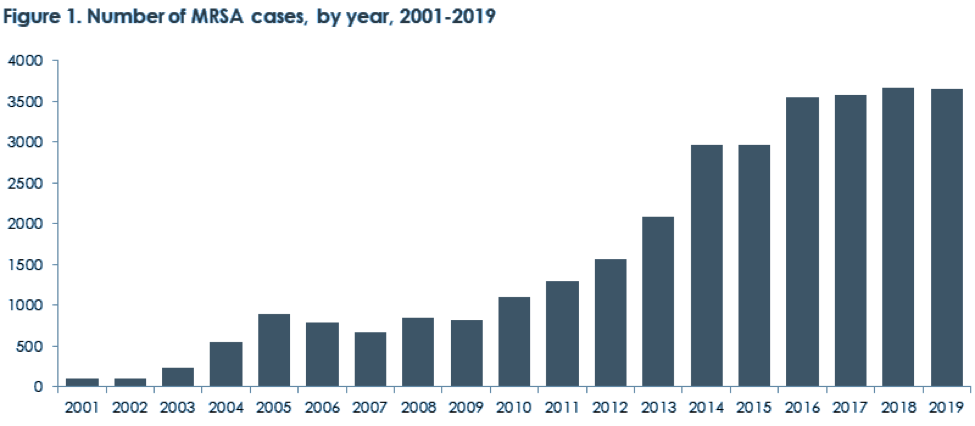
Figure 1: Number of MRSA cases from 2001 – 2019 in Denmark2
The Staphylococcus aureus bacteria can enter the human body either by
- Hospital onset: The bacteria is acquired by the patient either during or after a hospital stay, or after a medical device implantation.
- Community onset: The bacteria enters the body through uncovered minor cuts or wounds. The infection is also spread through injection of drugs like opoids, etc.
Clinical manifestation of a Staphylococcus aureus infection
A Staphylococcus aureus infection is a leading cause of various diseases such as
- Bacteremia and sepsis – When the Staphylococcus aureus bacteria enters the bloodstream, the body fights the infection and damage its own tissues. Sepsis kills about 30 to 50% of people post-infection3.
- Infective Endocarditis – The bacteria infects the heart lining, heart valve or the blood vessels.
- Surgical site infections – Almost 20% of surgical site infections are caused due to the Staphylococcus aureus bacteria4.
- Toxic Shock Syndrome – The entry of Staphylococcus aureus bacteria into the bloodstream causes toxins due to the overgrowth of bacteria. The mortality rate of Toxic Shock Syndrome due to a Staphylococcus aureus infection is 5 to 15% 5.
- Pneumonia – The Staphylococcus aureus bacteria infects people with an already existing lung condition and causes pneumonia.
- Osteomyelitis is a bone infection that is caused due to the staphylococcus aureus microorganism leading to bone destruction and loss.
The Staphylococcus aureus bacterial infections are difficult to treat because the bacteria acquires resistance against certain antibiotics. The infection is caused by different types of staphylococcus aureus microbes such as methicillin resistant staphylococcus aureus (MRSA), methicillin-susceptible staphylococcus aureus (MSSA), etc. The most common microbe is MRSA and is deadly than other staphylococcus aureus infection. The mortality rate of an MRSA infection is 21.8% 6.
With such an alarming mortality rate due to Staphylococcus aureus infection, it is very essential to quickly identify the staph aureus infection and start with the right set of antibiotics as early as possible.
Detecting a Staphylococcus aureus infection
The detection of a Staphylococcus aureus infection rapidly is of paramount importance once the Staphylococcal aureus enters the bloodstream and can become life-threatening.
Once a physician suspects a Staphylococcus aureus infection, the physician takes blood from the patient and tests for the Staphylococcus aureus infection.
The conventional bacterial culture method uses blood or other body fluids to detect the presence of Staphylococcus aureus infection. The time of detection varies from 2 to 7 days and the sensitivity is also quite low. So this method is not good for rapid identification of the Staphylococcus aureus infection.
Several immunological methods can also detect a Staphylococcus aureus infection. These methods use immunological reagents to detect the specific proteins in bacteria. The immunological methods often offer very poor sensitivity of only 12-80%. A more recent Staphaurex Plus kit recognizes the capsular antigen and also the clumping factor but sensitivity was as low as only 23%13.
Biochemical tests such as Coagulase test is used to identify and differentiate Staphylococcus aureus infection from other Staphylococcus species infections. The coagulase test is not very promising method as false positive results may occur and time taken for the positivity is at least 24 to 48 hours. Also the sensitivity of this method is as low as 79.5%14.
Molecular biology tests such as Real-time Polymerase Chain Reaction has the potential for accurate and rapid identification of Staphylococcus aureus infection. FDA has approved 2 PCR-based assays developed by BD diagnostics and Cepheid to detect Methicillin Resistant Staphylococcus Aureus infection. But these real-time PCR tests have a high rate of false positives upto 7.7% and also fail to detect emerging new strains12. All contemporary methods of detection of a Staphylococcus aureus infection are summarized below.
Detection method | Method | Advantages | Disadvantages | Time taken for the result |
Bacterial Culture7 | Specimen from blood, body fluids are cultured and grown under ambient conditions for bacterial growth | Cost effective
|
| 4 to 7 days |
Immunological Procedures8 |
| Shorter detection time compared to blood culture methods |
| 24 to 48 hours |
Coagulase test | Differentiates other staphylococcus species from Staphylococcus aureus bacteria |
| 24 to 48 hours | |
Real-time PCR |
|
| 24 hours |
Table 1. Different detection methods along with advantages and disadvantages
As you can see most existing detection methods pose many challenges such as lacking selectivity, sensitivity or speed. Micronbrane addresses issues above with its novel mNGS-based assay called PaRTI-Seq® that incorporates patented technology of host DNA depletion with Devin® filter. Devin® filter membrane utilizes Zwitterionic interface Ultra-Self-assemble Coating Technology (ZISC Technology) that in just 5 minutes depletes 95% of human nucleated cells. Samples pre-processed with Devin® filter have much higher microorganisms’ enrichment and thus provide higher percentage of sequencing reads in comparison with other depletion methods.
PaRTI-Seq® (Pathogen Real-time Identification by Sequencing) is a proprietary technology built upon Devin® filter, in-house database and bioinformatic analytical software, which optimizes the whole workflow of pathogen detection and make it possible to get full pathogens report within 24 hours upon sample arrival. Moreover, with Devin® filter full cost can be optimized in least twice as PaRTI-Seq® requires much fewer sequencing reads to identify pathogens in the sample. You can learn more about advantages of this technology in the latest paper Novel Cell Depletion Method Enables Pathogen Identification by NGS.