Are you coughing, sneezing, having a mild fever, and feeling a little tired?
These symptoms can be from allergies or a common cold. Still, there is a risk that they may be due to a respiratory infection because the respiratory tract is the most common route of microbial entry. Early diagnosis and treatment of respiratory diseases can be life-saving. Sometimes, respiratory infections (pneumonia, tuberculosis) can be life-threatening if not diagnosed and treated promptly.
What are Respiratory tract infections?
Respiratory tract infections (RTIs) affect the respiratory system, especially sinuses, throat, lungs, or airways. According to the Global Burden of Disease(GBD) studies conducted in 2013 and 2015, RTIs are the primary cause of life-threatening respiratory disorders and are considered the third most common health issue for international travelers. Similarly, World Health Organization (WHO) child mortality data published in 2018 reported that respiratory infections are one of the leading causes of childhood morbidity and mortality. Recently, a published study regarding the global burden of respiratory infections in 204 countries and territories (from 1990 to 2019) reported that “RTIs are highly prevalent globally, especially in developing countries”.
Respiratory infections are divided into the upper respiratory tract (URTIs) and lower respiratory tract infections (LRTIs), based on the area of the respiratory system they affect.
Upper respiratory infections are one of the most common reasons for doctor visits.
The upper respiratory tract includes the sinuses, nasal passages, pharynx, and larynx. Upper respiratory tract infections are contagious and refer to acute illnesses of sinuses and the throat. Some common URTIs are common cold, influenza, sinusitis, tonsillitis, laryngitis (inflammation of the larynx), pharyngitis (inflammation of the pharynx, uvula, and tonsils, also known as a sore throat), epiglottitis (inflammation of the upper portion of the larynx or the epiglottis) and laryngotracheitis (inflammation of the larynx and the trachea), and tracheitis (inflammation of the trachea). There is a significant overlap in symptoms of allergy and acute respiratory infections. During URTI, mostly patients experience varying symptoms ranging from the common cold, stuffy nose, cough, nasal congestion, sore throat, sneezing, and mild fever.
The lower respiratory tract includes infections that affect the lower airways, such as the trachea and lungs. Common LRTIs includes pneumonia (hospital-acquired and community-acquired), bronchitis, bronchiolitis, tracheitis, and tuberculosis. According to the United Nations Children’s Fund (UNICEF), only pneumonia accounts for almost 15% of deaths of children aged under five.
Common Pathogen causing Respiratory Tract Infections
Respiratory tract infections are caused by numerous pathogenic organisms, including bacteria, viruses, and fungi, presenting vague clinical symptoms. The majority of the respiratory infection cases are caused by viruses such as influenza A and B, respiratory syncytial virus (RSV) A and B, parainfluenza virus types 1–3, adenovirus, rhinovirus, human metapneumovirus (hMPV), and others. According to the world health organization, about 90% of upper respiratory tract infections and 30% of lower respiratory tract infections are caused by viruses. Several different viruses can cause each respiratory syndrome, and each virus can result in several other clinical presentations. Common viruses that cause upper and lower respiratory infections are mentioned in Figure 1.
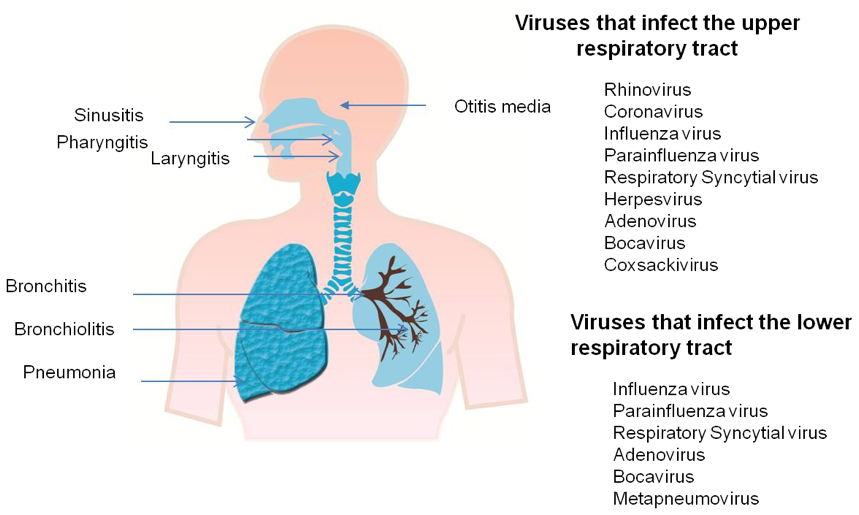
Figure 1. Common upper and lower respiratory tract viruses
Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis mainly cause upper and lower respiratory bacterial infections. Streptococcus pyogenes is the primary bacteria causing pharyngitis and tonsillitis. Microbial agents causing atypical pneumonia are Mycoplasma pneumoniae, Chlamydia, Legionella, and Coxiella burnetti. Bacteria causing upper and lower respiratory infections are listed in figure 2.
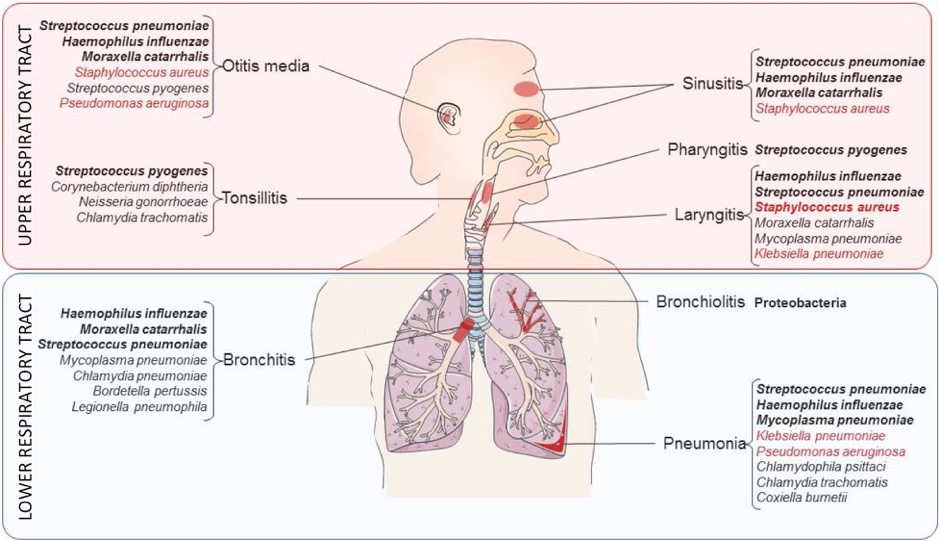
Figure 2. List of the bacteria responsible for upper and lower respiratory tract infections
Mostly respiratory infections do not need any treatment, and patients get better by following home remedies. Still, sometimes they get abruptly worse, and patients need to visit a physician for immediate proper treatment.
Fighting Respiratory Infectious Diseases with Molecular Diagnostic Tests
Early diagnosis, mainly the rapid and accurate identification of the causative pathogen, is critically important to cure the disease. Generally, medical history and detailed physical exam are combined with different tests to diagnose respiratory illness. Mostly performed tests are bronchoscopy, pulse oximetry, nose swab, chest X-rays, blood or mucus tests, CT scan, tuberculin skin test, spirometry, and peak flow meter. However, there is a lack of specific tests to identify all potential microbes in acute respiratory tract infections. All available microbiological diagnostic tests are slow and have some limitations related to specificity and sensitivity.
In the last decade, there has been a notable development in diagnostics of respiratory diseases, with the availability of advanced molecular assays. Molecular diagnostic methods, such as direct immunofluorescence assays and nucleic acid amplification technique using polymerase chain reaction (PCR), have improved the sensitivity, specificity, and rapidity. Even though new molecular methods offer higher sensitivity and specificity over conventional gold standard methods, they still require prior knowledge or assumptions regarding the types of pathogenic microorganisms11.
Role of next-generation sequencing in the detection of respiratory pathogens
Diagnostic assays based on sequencing are developing and becoming more sophisticated over time. In advanced next-generation sequencing-based protocol, it is possible to identify all the microbes in a given sample using NGS. Next-generation sequencing platforms, particularly metagenomic next-generation sequencing (mNGS), are potential diagnostic tools for faster and reliable microbe identification. The significant advantage in mNGS is the unbiased sampling, which allows the identification of all potential microbes simultaneously.
Table 1. Comparison of different diagnostic methods for Respiratory tract infections (RTIs)
| Diagnostic Test | Advantages | Limitation | Cost |
| Culture |
|
| Low |
| Serology |
|
| Low |
| Nucleic Acid Amplification Assay (Direct, Multiplex & Targeted universal multiplex PCR) |
|
| Medium |
| mNGS |
|
| High |
PaRTI-Seq® (Pathogen Real-Time Identification by Sequencing) by Micronbrane Medical addresses the major bottleneck of all mNGS techniques with its novel device Devin® and provides an easy and fast method to detect specific pathogens within 24 hours. Membrane filter Devin® depletes human host DNA, enrich microbial organisms in the sample and thus reduces output for downstream sequencing, making pathogen identification less time-consuming and more cost-effective. You can read more information about Devin® and PaRTI-Seq® here.
References
- Abdulmuhsin Mohammad K. Global regional and national life expectancy all casue mortality and casue specific mortality for 249 causes of death. The Lancet. 2016;388(10053):1459-1544.
- Abubakar I, Tillmann T, Banerjee A. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117-171.
- Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. The lancet. 2012;380(9859):2095-2128.
- UNICEF. Levels and trends in child mortality. 2018 Report. Estimates Developed by the UN Interagency Group for Child Mortality Estimation. 2019.
- Jin X, Ren J, Li R, et al. Global burden of upper respiratory infections in 204 countries and territories, from 1990 to 2019. EClinicalMedicine. 2021;37:100986.
- Cilloniz C, Martin-Loeches I, Garcia-Vidal C, San Jose A, Torres A. Microbial etiology of pneumonia: epidemiology, diagnosis and resistance patterns. International journal of molecular sciences. 2016;17(12):2120.
- Wardlaw TM, Johansson EW, Hodge MJ. Pneumonia: the forgotten killer of children. Unicef; 2006.
- Cruz AA. Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach. World Health Organization; 2007.
- Nair H, Nokes DJ, Gessner BD, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. The Lancet. 2010;375(9725):1545-1555.
- Thornton HV, Blair PS, Lovering AM, Muir P, Hay AD. Clinical presentation and microbiological diagnosis in paediatric respiratory tract infection: a systematic review. British Journal of General Practice. 2015;65(631):e69-e81.
- Das S, Dunbar S, Tang Y-W. Laboratory diagnosis of respiratory tract infections in children–the State of the Art. Frontiers in microbiology. 2018;9:2478.
- Noviello S, Huang DB. The basics and the advancements in diagnosis of bacterial lower respiratory tract infections. Diagnostics. 2019;9(2):37.